That’s the question we put even if we haven’t been diagnosed with depression. We may find ourselves in moments that seem to never end or come back too often. Well, it’s not your fault. And by “you” I mean your thoughts, emotions or actions.
Your physical body may be the one to blame.
Have you ever heard the concept that our gut is our second brain? I personally am rather surprised of how much we depend on this GUT. And if you wonder why you are depressed all the time, then your gut bacteria may be the answer.
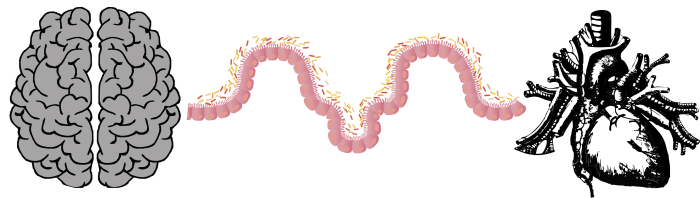
We call our intestines the second brain. An we also say “A man’s love comes from his stomach”.
It seems that our digestive/intestines rule the 2 most important parts of our life: emotion and conscious. How strange is that!
Depression is one condition that affects both emotions and conscious. And, guess what! Science has just proved that depressed people are missing certain important bacteria from their gut! Microbiota and mental health are again connected.
Haven’t I told you already that we are not in control of anything? That we are like puppets in our hormone’s hands ?
Jeroen Raes of KU Leuven University in Belgium and colleagues examined over 1000 volunteers in Belgium who’d had the bacteria living in their gut genetically sequenced.
The team found that two kinds of bacteria, Dialister and Coprococcus, were less common in people who reported that they were depressed. The same result was seen in a second group of over 1000 volunteers from the Netherlands.
Of course nobody believes that lacking these 2 bacteria causes depression. But it is hilarious to say that people with depression eat differently and that this changes their gut flora. Because this was one possible explanation scientists came up with.
Really? Depressed people eat differently? Like what? Hamburgers, chocolate, coke? Of course, and all the rest of the people eat only vegetables, exercise every day, meditate and just feel happy and fulfilled every day of their life! omg…
So, starting from the idea that depressed people eat stuff that kill the 2 good bacteria, scientists tell us that both these bacteria make an anti-inflammatory compound called butyrate.
And so we come back to the bad influence inflammation has upon depression.
But it seems to me that depression is more recognized as a condition of the whole body, not only as a mental disease.
Depression, as a cumulus of thoughts, emotions, general behavior, is just a side-effect.
On the other hand, it was also recognized that emotions can directly affect stomach function. So the circle is complete. Unfortunately.
Ever since 1915, influential physiologist Walter Cannon noted that stomach functions are changed in animals when frightened. The same is true for humans. Those who stress a lot often report diarrhea or stomach pain.
The brain communicates with the gastrointestinal system.
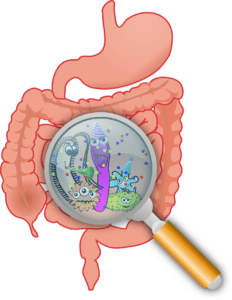 Our bowls represent a whole ecosystem comprising 100 trillion bacteria living inside them. (are they the ones chatting with our brain?)
Our bowls represent a whole ecosystem comprising 100 trillion bacteria living inside them. (are they the ones chatting with our brain?)
As a funny thing, today doctors are trying to heal the gut starting from the brain. They recommend talk therapy and antidepressants as possible treatments for symptoms of chronic gut problems!
Talk to the brain to talk to the bowls and fix their problems!
I wonder if the vice-versa is possible. We start from the missing 2 bacteria, ingest tons of them and then heal the brain. Wouldn’t his be great?
Studies also suggest that those with anxiety and depression are more likely to develop bowel disorders.
Is the brain that drives gut symptoms, or the other way round?
To see if the gut dysfunction precipitates the central nervous system features such as anxiety, or it was the brain that triggered the gut dysfunctions, an Australian team of researchers conducted by N A Koloski, made a 12-year prospective population-based study.
Here are the results:
| Baseline | 12 years later |
| 1. no gut problems + high anxiety (no depression)
2. gut problems + no anxiety or depression |
1.developed gut problems
2. developed anxiety and depression |
Higher levels of anxiety and depression at baseline were predictive of IBS at follow-up;
depression was predictive of FD at follow-up.
How can the brain possibly talk to the bowels?
Scientists tell us something as loosely as possible: through a network of neural, hormonal and immunological messages. We come back to our tenants, the bacteria.
Stress can influence the type of bacteria inhabiting the gut, making our bowel flora less diverse and possibly more attractive to harmful bacteria (Michael T. Bailey, 2011). It can also increase inflammation in the bowel (Bruno L.Bonaz et al, 2012), and vulnerability to infection.
So, every time you are under stress you alter the bacteria. This may lead to inflammation and chronic intestinal inflammation may lower our sensitivity to positive emotions, our brains become rewired (Alessandro Agostini et al, 2011) through a process called neuroplasticity, which changes the connections between the nerve signals. Complicated, I know.
Anxiety and depression are common in people suffering chronic bowel problems.
20% of those living with inflammatory bowel disease report feeling anxious or blue for extended periods of time (Antonina Mikocka-Walus et al., 2016) . In disease flares, this rate may exceed 60%.
Irritable bowel syndrome and depression
48 clinical trials confirmed that talk therapy and antidepressants improve bowel symptoms. This was shown in a systematic review and meta-analysis conducted by A C Ford and his team, ever since 2008. So, why in 2019, when I go to complain about my bowl problems, my doctor doesn’t say anything about this?
I wonder is he doesn’t trust these results or simply does not know about them.
But my doctor does mention good bacteria.
Only that he doesn’t know that the lack of it may very well be caused by stress. And then, going round and round, the lack of good bacteria affects our mood, sleep and stress levels. 🙁 It seems like there is no way out of this.
And yes, if we take bacteria from the gut of a depressed people and place them in the gut of a healthy one, the latter will develop depression as well.
In the study Transferring the blues: Depression-associated gut microbiota induces neurobehavioural changes in the rat., by Kelly JR et al.from 2016, 34 patients with major depression and 33 matched healthy controls were recruited to show this on mice. The researchers prepared a fecal microbiota transplantation from a sub group of depressed patients and controls and transferred by oral gavage to a microbiota-deficient rat model.
The ressults whowed that fecal microbiota transplantation, from depressed patients to microbiota-depleted rats, can induce behavioural and physiological features characteristic of depression in the recipient animals, including anhedonia and anxiety-like behaviours, as well as alterations in tryptophan metabolism.
Here is a very good video I found on youtube, which tell us what everything we need to know about bacteria.
References:
People with depression are less likely to have certain gut bacteria